The information provided on this page is available to download as a printable booklet. If you would like to view this page in Welsh please click here.
A person living with dementia will often experience problems controlling the function of their bladder (urine, pee) and bowel (faeces, poo) at some point. This is often referred to as continence (or incontinence).
This can take many forms. It may be short term because of problems with physical health. Some people may just need help finding the toilet and can manage with minimal assistance. Some people in more advanced stages of dementia may have considerable problems managing going to the toilet.
By supporting the person you care for to manage their own continence for as long as possible, you will help preserve their dignity, sense of control and quality of life. To do this it is important to take time to learn, plan and find out what works best for you both.
This page provides guidance and practical tips on supporting the person with their toileting needs, reducing the risk of accidents (soiling) and ensuring comfort and well-being.

This page covers:
- Establish a routine
- Making it easier to use the toilet at home
- Assisting a person to use the toilet
- Supporting a person who can no longer use the toilet
- Continence products
- Care at home to cope with continence needs
- Using the toilet when out and about
- Food and drink to help bladder and bowels
- Common health conditions that can lead to changes in bladder or bowel habits
- Getting help with continence issues
Establish a routine
People often develop their own natural toileting routines over a lifetime, so understanding these patterns can be helpful in providing effective support.
- Try to get to know the persons usual habits. Does the person tend to go to the toilet as soon as they get up in the morning, after meals and hot drinks, or before bedtime?
- People’s habits can change progressively as they age in that people often report needing to get up in the night to use the toilet.
- Having a warm drink in the morning can sometimes stimulate the need to open the bowels and may be useful in establishing a routine.
- Creating a timetable for yourself with reminders of when the person usually needs the toilet or setting an automatic alarm can help here.
- However, each day may present new challenges and sometimes a strategy that has worked perfectly well on previous occasions has the opposite effect at other times.
- Sudden changes in habits may be due to physical illness.
Making it easier to use the toilet at home
There are several practical things that can be done to help the person you care for manage their own continence at home.
- Finding the way to the toilet or bathroom can be challenging for the person with dementia. This is particularly the case if you have moved to somewhere new. The section on disorientation may be useful.
- A simple sign or picture on the toilet door, that is easily visible, can help.
- Simply leaving the door to the toilet open so that the person can see it can also help.
- Make sure the route to the toilet is free from clutter and trip hazards and is well lit, especially at night, to avoid falls.
- Dementia can affect a person’s ability to distinguish things that look similar such as toilets and wash hand basins. If possible, use contrasting colours to make key features, like the toilet seat or grab bars, more visible.
- If this is a problem, covering the sink with a towel when the person needs to use the toilet may help prevent confusion.
- If the person you care for becomes less mobile or tends to lose their balance, grab rails, a raised toilet seat and non-slip mats can make it easier to sit down and stand up independently and safely.
- A commode and/or a portable urinal may help when getting to the toilet becomes too difficult, especially during the night.
- An Occupational Therapist can provide guidance on equipment.
- Clothing with easy-to-use fasteners or elastic waistbands is easier to get on and off, and up and down.
- Keep toiletry supplies, like toilet paper and wipes easily accessible.
- Consider using brightly coloured hand soap to help with hand washing after using the toilet.
- It’s not uncommon for individuals with dementia to hide wet or soiled clothing or bedding out of embarrassment. Approach the situation with compassion and understanding. Avoid expressing frustration or blame, as this can increase feelings of shame and anxiety.
- If the person you care for continues to hide wet or soiled clothing, gently investigate the reasons behind this. It may be helpful to consult a healthcare professional or dementia specialist for further guidance and support.

Assisting a person to use the toilet
As a person’s dementia progresses, their ability to recognise the physical signals that they need the toilet may diminish. The person you are caring for may not be able to identify where the toilet is or how to use it. If this happens, they will need your additional support using the toilet, managing unavoidable accidents, and making sure their skin is clean and dry.
A referral to the local Bladder and Bowel Health (Continence) NHS Service can provide a specialist assessment and a personalised plan. This will include a review of what medications the person is taking and if they may be making the continence worse.
They will also check whether there might be another reason for the person’s change in bladder or bowel continence that could be addressed.
The following short clip may be of interest. Di shares her experiences of supporting her mum with using the toilet.
Top tips for helping someone use the toilet
- Find words and phrases for going to the toilet that work for your both. These might be familiar family favourites like ‘spending a penny’ or ‘having a pee and poo’.
- It can also help to break down instructions into small steps, provide gentle reminders if necessary and maintain a calm and reassuring tone to avoid causing distress.
- If the person you care for is not able to verbally communicate the need to go to the toilet, watch for signs like fidgeting and pulling at clothes.
- Consider how long someone can hold on between knowing they want to go to the toilet and starting to pee. This may allow sufficient time to get the person to the toilet and to help them remove their clothes. The easy on and off clothes mentioned previously will help too.
- Try prompting them to hold on until they are in the right position before they start to pee.
- Some people may not be able to hold on at all. Having a change of clothes at hand can help minimise embarrassment if this occurs.
- Once settled, give the person time without feeling rushed. It may take a little time for things to get started. Step away for a few minutes or stand nearby, just outside the door, and return when they’re ready.
- When ready, hand the person toilet paper to use as needed. You may need to help get the person started.
- Using wipes can sometimes be easier than toilet paper if you need to wipe for them. When wiping the person’s bottom, wipe from front to back which helps prevent bladder infections.
- In some cultures, it is normal to wash after wiping when you go to the toilet. If that is the norm for the person in your care, make sure there is a utensil such as a small plastic jug or bottle available by the side of the toilet that can be easily used to pour water when washing after using the toilet.
- Hygiene is very important when helping someone to use the toilet. Washing hands before and after will help to minimise risk of infection. Some people may prefer to use disposable gloves and aprons, which can be purchased from chemists or online.
The DemCon website developed by researchers at Southampton and Kings College London offers information for people living with dementia, friends and family carers, professionals and home care workers.

Supporting a person who can no longer use the toilet
Some people who are living with advanced dementia or who have other health issues may no longer be able to control their bladder and bowel function. A referral to the local Bladder and Bowel Health (Continence) NHS Service can provide a specialist assessment and a personalised plan. Additional support will also involve making sure the persons skin is clean and dry after using the toilet or soiling. This is especially important if the person is using continence pads or pants.
- The personalised plan may also include continence products like absorbent pads or underwear, and bed/chair protection such as absorbent mats and waterproof sheets.
- These products are designed to manage bladder and bowel incontinence discreetly and effectively, allowing the person you are caring for to remain active and engaged in daily activities.
- If you initiate the discussion about wearing incontinence products, allow the person you support to express a range of emotional reactions initially.
- When responding to their specific concerns try to be honest and factual e.g. “Yes the pads inside your pants will feel a bit bulky/ different at first.”
- Try to remain positive, you could say things like, “We can try different sizes and shapes of pads to suit you, it will mean we can enjoy a more relaxed walk to the shops together.”
- To prevent sores and infections gently wipe the skin with mild soapy water. If the person does not like the sensation of water against their skin, then try wet wipes or cleansing foam.
- Cleansing foams and wet wipes can be used without water. Ask your pharmacist for more information on suitable products.
- Then pat the skin dry, don’t rub as this can damage the skin more.
- After cleaning, ensure the person’s skin is completely dry before applying any protective creams or products.
- Try not to overapply though, as thick creams can affect the absorbency of pads and may cause more skin soreness.
- Dispose of used pads by placing them in a disposal bag or a suitable container and throw them away as soon as possible. Enquire about collection services provided by your local council as they may offer this service.
- Some people find it easier to provide continence care using disposable gloves and aprons, which can be purchased from chemists or online.
- Keep an eye on the quantity of urine that is being absorbed by the pad. If you are concerned that pads are frequently dry, contact your GP to ensure the person you care for isn’t dehydrated or has other medical needs that need addressing.
Continence products
The variety of different continence products can feel a little overwhelming as there are so many products to choose from.
- The Bladder and Bowel Health (Continence) specialist team will be able to guide you and tell you if you are eligible for free NHS funded supplies. You can ask your GP for details of your local continence service.
- If the person you support regularly pulls out soiled pads from their pants you might want to consider purchasing continence products that better suit your needs, these may be in the form of more substantial pull-up disposable incontinence pants.
- Pull-up disposable pants are close fitting support pants with large integral area of shaped absorbent material and soft elasticated edges to prevent leakage.
- Rather than pulling down soiled pants, you can tear each side of the disposable pants at the hips and remove the soiled pants in one movement. These products can be beneficial in maintaining dignity and comfort for a person whose continence is unpredictable or not well controlled.
- There are a variety of brands, sizes and absorbency capacity on the market e.g. Boots, Tena etc.
- Many budget supermarkets also do very similar products at a lower price point.
The Bladder & Bowel UK organisation have a practical guide on incontinence pads and AgeCo focus on incontinence.
The following short clip may be of interest. Paul shares his experiences of supporting his wife with continence. The products he mentions are ones that he has found helpful, but should not be taken as an endorsement. Everyone needs to find the right products for their situation, bearing in mind any allergies or sensitivities.
Care at home to cope with continence needs
There may be occasions when, despite these practical tips and trying different approaches, care becomes difficult and you may meet resistance from the person you are caring for. If you are struggling, help is there. Seek advice from the Health Professional sources. This level of continence care is particularly challenging. Home care agencies can help here. Attendance allowance can help offset some of the costs associated with this.
Any adult in Scotland who the local authority has assessed as having personal care needs, is entitled to free personal care. This includes under 65’s, so relevant for people with Young Onset Dementia, however this is likely to be funded through Self Directed Support, rather than attendance allowance www.gov.scot
Using the toilet when out and about
Using unfamiliar toilets can be very stressful as they are generally not designed with people living with dementia in mind.
Difficult environments can include: motorway service stations and garden centres, which often have confusing layouts, and toilets may be hidden behind retail and food displays; Public toilets, where the design makes it difficult to distinguish door handles, taps and dryers; Electronically operated doors on public toilets and train toilets; Hospital and shopping centre toilets, which may have more than one entrance and exit; Toilets with locks that are not obvious how they open and close.
Top tips when out and about
- Try to plan ahead. If you are visiting a place for the first time, find out where the public toilets are www.toiletmap.org.uk
- Be aware of the gender and type of public toilet the person feels most comfortable with.
- If you need to help the person go to the toilet, check the Changing Places map for an accessible toilet.
- A Radar key is a specifically designed key that fits the majority of disabled toilets around most city and town centres. Get a Radar key for access to more than 10,000 disabled toilets across the UK from Disability Rights UK or the Blue Badge Company.
- If it is likely the person will need the toilet urgently, order a Just Can’t Wait card (this allows you to use any toilet in a restaurant or bar without having to make a purchase) from the Bladder and Bowel organisation.
- Some people may not be able to give more than a few seconds warning that they need to ‘go’ which can result in continence mishaps. Bear in mind that accidents are more obvious on light coloured clothing. Having an ‘emergency pack’ of a change of clothes and wipes in case this happens can be a good idea.
- When visiting a new pub, café or restaurant, telephone ahead and ask about the toilets:
- What is access like?
- Is there only one entrance/exit?
- Are there traditional doors, handles, taps and dryers? Or will the person need to be accompanied into the toilet to provide assistance?
- Can you book a table in line of sight of the toilets so the person will not get lost?
- If possible, go into the toilet first and check everything, including making a mental note of the type of door lock, so that if the person gets locked in, you can calmly help coach them how to unlock the door. This will save much embarrassment, and possible expense, at having to get the door removed.
In the following short clip Di shares her experiences of using toilets when out and about with her mum, reinforcing some of the top tips above.
Food and drink to help bladder and bowels
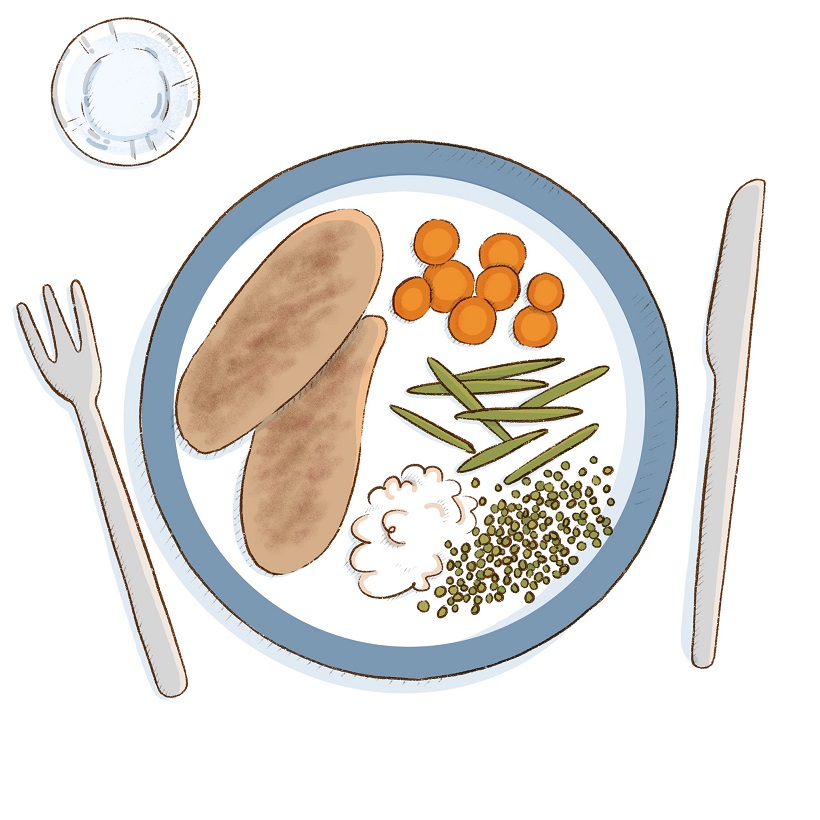
Having a balanced diet and drinking plenty of fluids are essential for keeping bowel movements (having a poo) regular and for reducing the risk of urine (pee) infections. It will also help to maintain the routine. To help this:
- Encourage a diet with plenty of high-fibre foods, fruit and vegetables.
- Whilst it’s natural to want to reduce drinks to cut the number of visits to the toilet, generally people are encouraged to drink 2 litres per day. Of course this will vary from person to person.
- Remember fluid is contained in all drinks and ice-lollies. Plenty of fluid will help keep the faeces/ poo soft and help prevent constipation and dehydration.
- If the person is able, encourage them to keep active as this helps with regular bowel movements.
Common health conditions that can lead to changes in bladder or bowel habits
There are many physical health problems that cause changes in bowel and bladder habits. Because of the communication problems and memory problems associated with dementia, the person may not be able to communicate directly about symptoms. Being alert to common symptoms of problems can help you to ask for help.
Constipation
Be alert to signs of constipation which may include:
- Less frequent bowel movements (not having a poo at least 3 times a week or pooing less often than usual).
- Straining or pain when having a poo.
- Smearing or liquid poo. This may mean there is a hard constipated poo higher up the bowel, which leads to liquid poo leaking out around it.
- Abdominal or tummy discomfort.
- Loss of appetite.
- Worsening confusion or irritability.
Urinary tract infections
Be alert to signs of urinary tract infections (UTI) or bladder infections (cystitis), which may include:
- Needing to pee more often the usual, and without much warning.
- Pain or burning when peeing.
- Abdominal or tummy discomfort.
- Sudden and increased confusion, agitation, or withdrawal.
- Flu-like symptoms such as high temperature, aches and pains.
Other conditions
- Some commonly prescribed medications can make the person want to pee more or worsen constipation. It is worth discussing this with a doctor or pharmacist if you think this may be an issue.
- Medication, such as iron tablets for example, can also change the colour and consistency of poo so you may find there are changes to toilet habits when medication is changed. If you haven’t been made aware of this beforehand, consult your doctor if this happens to check that the changes are a recognised side effect or whether it needs further investigation.
- Problems with the prostate (in men) or prolapse (in women) can also cause problems.
If you have concerns that the person you care for may have these symptoms, contact the GP or community nurse as soon as possible.
Getting help with continence issues
Many people are embarrassed when talking about continence. It is often surprising how many people have issues with continence. There are many different health and care professionals that can provide practical advice, equipment and aids.
- GP: They can assess and advise regarding changes in health. They can refer onto specialist NHS services.
- Bladder and Bowel Health (Continence) Service: They provide a specialist assessment and a personalised plan for people with complex continence needs and advise about pads and continence aids.
- Clinical Psychologists can help with assessing abilities and understanding of whether the person has perceptual problems by offering a neuropsychological assessment. They can also help with understanding how you can support someone who is becoming distressed on a regular basis. A GP can make a referral for this service.
- District and Community Nurses: These teams are often linked to GP surgeries. They provide advice and treatment to patients at home for a range of needs including continence care.
- Community Mental Health Nurse (sometimes called Community Psychiatric Nurses or CPNs): These are specialist NHS nurses who support and advise people with dementia and have specialist skills in managing distress and difficulties. They work within the specialist community mental health team for older people which will include psychiatry and psychology.
- Social worker: They work for the Local Authority in the department of Adult Social Care and deal with all aspects of social care. They can help if you need help at home. They will undertake financial assessment to advise on the cost of this. They also advise where there is a risk to safety to individuals living with dementia.
- Admiral Nurses: They are specialists in the care and support of people and families affected by dementia. Some NHS Trusts have Admiral Nurse services where you can call directly. Their free help line can offer direct advice from Admiral Nurses about continence issues and dementia 0800 888 6678
- Occupational Therapist (OT): They can assess and help with specialist equipment that can make it easier to manage at home. They work either for the NHS or social services and referral is usually through your GP. Some work in private practice.
- Physiotherapists (Physio): can assess and help with movement, pain management and muscle strength. They work for the NHS and referral is usually through your GP. Some work in private practice.
- Pharmacists: They usually work in Pharmacies and are specialists in the use of all medications. They can offer free advice on which medicines are likely to impact on the bladder and bowel.
For advice and support phone any of these helplines: Alzheimer’s Society 03331 503456; Alzheimer Scotland 0808 808 3000; Dementia UK 0800 888 6678; Dementia Carers Count 0800 652 1102. Nothing that you discuss will shock or embarrass people on the other end of the phone.
