The information provided on this page is available to download as a printable booklet.
Over time there are a number of things that can help you continue to care for a person living with dementia in the longer term. This page includes issues and strategies that carers tell us they find useful.
This page covers:
- Aids and equipment
- Caring across cultures
- Dignity
- Gadgets (assistive technology)
- Medications
- Physical activity
- Music
- Preparation of personal care tasks
- Routines and order of routines
- Time
Aids and equipment
Aids and equipment include items such as toilet frames, shower chairs, bed rails, dressing aids, special drinking and eating cutlery, adaptive clothing, walking frames, wheelchairs, portable ramps. For some people, they can maintain health and well-being, and contribute to safety, independence, quality of life, and personal dignity.
This is not a one size suits all issue. Different aids will suit different needs and be appropriate at different times. A person with dementia may need a considerable amount of time to get used to using this type of equipment.
Various professionals such as Occupational Therapist (OT), tissue viability nurses, continence advisors, podiatrists and vision and hearing specialist can provide an assessment and access to relevant aids.
This ensures that the correct piece of equipment is chosen and that it can be used safely at home.
The OT or health care professional can assess, prescribe, and order some aids and equipment free of charge from the local Integrated Community Equipment Service (ICES). Many aids have to be paid for or have strict criteria on their availability. Other aids can be purchased privately. There are also adaptations and modifications that can be made to the wider home environment.

Top tips in using aids and equipment
- It is helpful to read reviews and feedback and think about whether the situation of other users is similar to your own.
- Talk to your dementia advisor, other carers or disabled living team for recommendations of reliable suppliers.
- It is also possible to get discounts/avoid VAT on some items if you’re in receipt of certain benefits such as attendance allowance.
- Carers online forums can be a useful place to pose questions and get feedback about items.
- It is a good idea to try out using aids and equipment before making expensive purchases.
- Some people with dementia may find it difficult to use a new device that they have not encountered before. Think about how you can introduce the aid and the best way to support the person to learn the new skills or routines that the new equipment requires. It is important to introduce it step by step, and one new thing at a time.
- It may also be useful to look at the section on gadgets.
Caring across cultures
If the person you are supporting has a different cultural heritage to yourself, it is important to understand what practices may be important to them in personal care. There are many things that are similar across different cultures, but some things may be different because of what is seen as the norm or expected. For instance, the person may enjoy music, but they may like different genres of music, music in different languages or of a different era. People often tend to enjoy music they know well from earlier times in their life – particularly their teenage years.
Similarly, there may be different preferences of how to take a shower or a bath. In some cultures, you do not sit in a bath of water. You have a shower or use a bucket and mug in the bath to put clean water over yourself.
Habits around using the toilet may also be different. For example, in almost all eastern cultures and faiths, people use water to clean or wash themselves after having been to the toilet, rather than just wipe clean.
In the West, people tend to eat with a fork in their left hand. In most eastern cultures people eat with their right hand. This includes people using a fork in their right hand when using a knife and fork.
These are important considerations if you are looking after someone from a different culture to yourself.
Some of us remember calling our parent’s friends ‘Aunties’. It is still common in many of our South Asian and Black communities to call one’s mother’s friend ‘Auntie’.
People don’t call older people by their names. They especially don’t use their first name unless given permission. There is also a cultural difference in how respect is given to an older person. We may want to encourage independence by asking an older person to help with tasks such as chopping or peeling vegetables to keep them busy or active in the home. In many families and cultures that is seen to be disrespectful – i.e. making them undertake ‘work’. It’s important to be sensitive and informed around how you encourage independence and activity.
Of course, some people do not follow cultural norms, so it is always good to ask the person in your care about their preferences, if they are able to tell you. The section on communication may help with this.
Dignity
Dignity means valuing the uniqueness of an individual, respecting their views and opinions, privacy and choices. The ability to look after oneself impacts on feelings of dignity. For many people with dementia, the decline in their ability to self-care can be very frightening, making them feel very vulnerable and isolated. This means they will often need a lot of support and reassurance to maintain their sense of dignity.
Top tips for maintaining dignity
- Taking a compassionate and co-operative approach can maintain dignity and respect.
- If a task does not need to be done at a particular time, consider whether it is doing more harm than good to continue. The section on washing and bathing may help with this.
- Good communication is crucial to maintaining dignity.
- If the person is treated with dignity and respect, they are more likely to comply with care.
- It is easy to make assumptions about how people wish to be treated. For example, it may be that they would be happier with a paid carer undertaking care activities with them rather than a member of their chosen family.
- Try to reflect regularly on what assumptions you are making and how the person is feeling.
- Having discussions early on in dementia can help clarify the person’s wishes and views on maintaining a sense of dignity.
- Respecting the person’s dignity in terms of preferred pronoun use can be important in building trust.
- Be ultra aware of protecting dignity by using coverings for the person’s body and always ask permission to support them with any aspect of personal care.
- When there are times when dignity has been compromised because of safety issues, ensure that an activity that builds the relationship back up happens soon afterwards.
- The LGBTQ+ Learning Framework contains useful information about supporting people: www.skillsforcare.org.uk
Gadgets (assistive technology)
Gadgets designed to help those living with dementia or their carers come onto the market very regularly. It can be difficult to navigate which are worth the time and the money.
Popular gadgets may be for collecting music playlists and playing music or films. Others may be devices to promote safety such as watches that identify somebody’s location or buzzers that sound if the front door is opened in a person’s home. Pressure mats and mattresses can sound an alert when someone gets up at night. Motion sensitive lights or door alarms for the bedroom, and falls alarms can help carers get rest at night whilst knowing they will be alerted if the person has got up to go to the toilet.
If the person with dementia lives alone or is home alone for periods of time, then an outside door alarm and/or camera can be helpful in addition to a key safe. The camera can alert the carer when someone leaves or enters the property. It also shows when healthcare or care visits to the home are occurring. Telecare/community call alarms can be helpful for some people. Find out more about Telecare alarms at www.telecare24.co.uk
An Occupational Therapist or trained professional can work with the person who has dementia and their carer to identify what assistance is required. Equipment is provided free in certain situations but it can also be loaned or bought.
Some gadgets can be very helpful but it really does depend on individual circumstances. What is tolerated or preferred by one person may not be liked by another. Some people living with dementia may embrace a new gadget such as a location device worn on their wrist. Others may find a wrist-worn device alien (in terms of size, weight, colour, material) if it is not like a watch or bracelet they are familiar with.
It is best to reflect carefully on gadgets with the person they are for and stick to known preferences. If someone never wore a watch before their dementia diagnosis, they may be reluctant to wear one once their condition progresses.
Devices such as sensors contained within clothing may be helpful for some but others may pull them out. It is difficult to ‘try before you buy’ from some sellers so look for providers through local services such as Occupational Therapists who can advise or provide some items.
Top tips for using gadgets
- Read reviews to help you think about whether a gadget is worth the investment.
- Carers forums can be a useful place to pose questions and get feedback about items.
- Some people with dementia may find it difficult to use a new device that they have not encountered before. Think about how you can introduce the aid and the best way to support the person to learn the new skills or routines that the gadget requires.
- If making a purchase, think about how the gadget will be used in months and years to come. Is its use very time-limited or a good long-term investment?
- Consider what is affordable to you and seek advice from others who may have used similar gadgets.
- Ultimately a gadget should be helpful in some way e.g. as an aide memoir, to help open something, identify something, as a reminder tool (such as to take medication), to organise (such as a daily pill dispenser) or can simply be a notebook to note visitors to the home.
- There are many resources and points of information about. You can find info on the following pages online:
- NHS www.nhs.uk
- NHSinform (Scotland) www.careinfoscotland.scot
- Age UK www.ageuk.org.uk
- Alzheimer’s Society www.alzheimers.org.uk

Medications
People with dementia can be prescribed lots of different medications which can be difficult to keep track of. Missing out on some medications can make providing support with personal care difficult. Likewise side effects and interactions between different medications can make caring much more difficult.
Top tips for managing medications
- A regular medication review is a good idea to make sure that people are not taking any unnecessary medications. Side effects and interactions between different medications can become a problem over time.
- If the person you are caring for is refusing to take medication that they need on a regular basis then you should seek advice from a health care professional – your GP usually in the first instance.
- Talk with the person about their medications so you can understand any issues that they may have about taking them.
- People with dementia and other conditions can have difficulty swallowing. Liquid or chewable versions of some medications are available and may be easier for the person. Patches are available for some medications.
- Speak to your pharmacist if you are unsure about how to give any new medication. They can advise you about sources of information for your device and condition. For example in using an asthma inhaler correctly there are some helpful videos on the Asthma and lung UK webpage www.asthmaandlung.org.uk
- Various weekly pill dispenser boxes (sometimes called dosette boxes) can help keep track of medicines to be taken at different times during the day.
- Prompting the person to take their medication at the right time is easier with a dosette box.
- A ‘Venalink’ medication system filled and dispensed by your local pharmacy, is a possible solution to achieving good medication routines. This makes it easier to see if the correct medication has been taken. Visit the Venalink website for more information www.venalink.co.uk
Physical activity
Many people have problems with movement generally because of general physical health issues related to getting older. What is good for the heart is also good for the brain. Staying physically active has many benefits for those living with dementia. This will bring all sorts of benefits in the longer term including better sleep, freer movement and greater feelings of wellbeing. The section on coordination may also be useful to consider in relation to physical activity.
Top tips for staying physically active
- Keep physical activities going where ever possible.
- Try to choose activities that the person enjoys, such as music and movement, walking with a dog, lawn bowling, social dance, swimming, gardening and different household chores. The key is movement with fun.

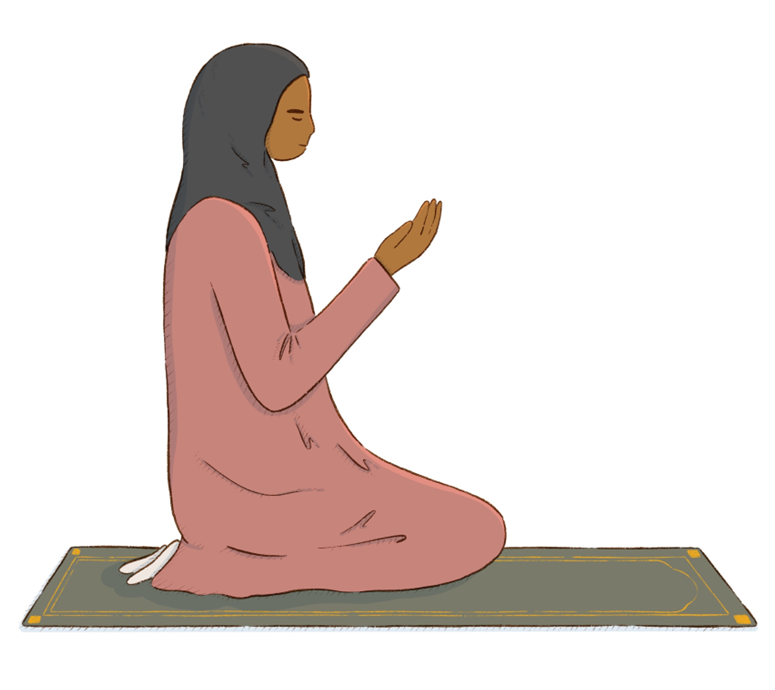
- Those who have been practicing their faith may still enjoy praying and going through the physical movements of prayer, e.g. standing, kneeling, bowing, prostration.
- For people with significant problems with movement, the advice of a physiotherapist and an Occupational Therapist can be useful.
- Health care professionals can also recommend treatments or interventions to improve movement such as exercise routines, referral to a medical practitioner if they suspect a treatable underlying cause for difficulty with movement.
- Health care professionals can suggest specific exercises for the person and techniques to help you when you are assisting the person to move around. They can also advise on the use of lifting equipment like a hoist.
- They can also refer to the local wheelchair service for the assessment and provision of a wheelchair and recommend different aids and adaptations.
Music
Music can be a highly valuable tool when supporting someone living with dementia. Incorporating music into the daily lives of those with dementia can have a positive impact on their well-being and overall quality of life. Music has the ability to evoke memories, stimulate emotions, and improve communication, providing a sense of comfort and familiarity. The use of familiar tunes and songs from the past can spark joy and connection. Music not only brings joy but also serves as a powerful tool in promoting relaxation, reducing anxiety, and improving mood.
Many carers find that incorporating music into personal care can be a positive experience.
Top tips for using music in personal care
- A music player in the room where you are providing personal care can be helpful.
- It may be a good activity to work together to create a playlist of music so that their favourite songs are easily accessible.
- If the person you care for prefers, you could try giving them a pair of headphones synced up to a phone or music player.
- You may find that this helps them relax so that they feel more comfortable with you helping them with their personal care routines.
- Try singing or humming along to favourite or well-known songs.
- Some people find that singing with or to the person they are looking after helps to create a lighter mood.
- In some communities ‘music’ may be vocal without instruments, such as prayers and recitation of scripture, whilst there is use of instruments in other faiths. For instance, Muslims listen or recite the Quran without music, but there is melody in the recitation, whilst in Hinduism and Sikhism there is usually musical instruments played alongside recital or singing. Whatever is the norm for individual will help them relate to it and find comfort listening to it.
- For some people, music can be overstimulating and attending to more than one thing at a time is difficult. Sometimes music can to too much of a distraction to focussing on personal care.
- Signs of overstimulation vary but if the person cannot focus or is closing their eyes or is looking tense, then turn the music off.
- See information by Dementia UK about the impact music can have on someone with dementia www.dementiauk.org

Preparation of personal care tasks
When undertaking any task that has several parts to it, we all make preparations to enable us to carry it out with ease and efficiency. For example, when following a recipe for a cake, ideally, we will have all the ingredients lined up and often in the exact amounts required so as to make the task easier.
When supporting someone with personal care, it is good to be prepared and have all you need to complete the task to hand. Try to avoid running around mid-task to look for something you have forgotten. It may be that you make the preparations to enable the person with dementia to do as much for themselves as possible, to maintain autonomy and independence for as long as possible. It may also support a person to undertake their own personal care by maintaining routines.
If there are items missing that are essential to undertaking a personal care task it can break the momentum and the task may not be completed because of an interruption to go and get something. Similarly, if the person you care for are more dependent upon you for care then having to leave them, perhaps in the shower whilst you leave the room to get a full bottle of shampoo, could present risks, such as their falling in the shower.
Top tips for preparation of personal care tasks
When making preparations for a personal care task, ensure that all the necessary things are in place at the sink or wherever is the usual place to do this.
- For example, if supporting the person to change an incontinence pad, ensure all the items you need are to hand so you can complete the task as quickly and as efficiently as possible.
- Lay out the items, i.e. clean pad and underwear, wash cloths, warm water, towels, etc.
- Preparation may also involve telling the person that you will be helping them with a particular personal care task, for example, to have a shave.
- If you do the same activity at the same time, this will aid as a prompt for the person as well, such as standing at the sink to both clean your teeth.

- It is important that you include explanations in both your planning and carrying out of care tasks, talking them through both what is happening as well as what will happen next.
- Preparing for managing care needs on trips outside the home is also important. Checking that there is access to suitable toilet facilities, and taking a change of clothes and extra supplies can save potential embarrassment and upset.
Routines and order of routines
We all develop our personal routines and an order in which we do our personal care throughout our lives. When we were children, this was influenced by our parents. When we are in education and working, our routine is influenced by timeframes that enable us to be prepared for the day. These patterns can become so established that we do not have to give them much thought and almost become ‘second nature’.
When a person develops dementia some of the routines, their order and coordination of personal care can become disrupted. They may need extra and increasing amounts of support from those around them. Establishing a consistent daily routine can help people feel more secure. An example of this might be washing your face before you clean your teeth, and always putting the toothpaste on the left hand side of the sink so it can be easily found.
Regular routines can also support better sleep patterns and overall well-being. For example, this may include having a regular time for going to bed, and listening to some calming music about half an hour beforehand. Familiar activities and routines can trigger positive memories and associations, giving a sense of comfort and stability.
Top tips for using routines
- Try, where possible, to follow the person’s established routines and order of routines, if you know what they are.
- If you are unsure, then have a period of working out what works best for the person you are supporting.
- Some people like to shower first thing or bathe in an evening. Some people may like to clean their teeth before they have breakfast and others may after a meal.
- Try to build a picture up of what their preferences are. This will help with following natural routines as you care for them.
- Part of supporting routines is avoiding going too fast for the person. Extra time and prompting may mean that the person can achieve tasks to their satisfaction at their own pace.
Time
Time often becomes a precious resource for a carer. A person living with dementia may lose their sense of time. They may experience problems being able to tell the time and may also experience timeslips where the person thinks they are in another era in their life.
Memory loss can then add to these situations, making multiple reminders part of a carer’s day. All of these factors can make it difficult when scheduling personal care activities.
As a carer you may feel that you know what time meals, getting up, going to bed, getting ready to go out etc. should be occurring. Disagreements over whether it is the right time for these activities can be very wearing.
Dementia often causes difficulties for the person both in terms of orientating themselves to the day, month year or season and with respect to understanding the passage of time. This ability to understand and manage time varies from person to person and may change as someone’s dementia progresses.
While there are no guaranteed interventions to help with this, there are a number of things that are worth trying out.
Top tips for helping the person keep track of time
- Try keeping clocks with clear faces around the home.
- Some people prefer analogue clocks with others finding digital clocks easier to read.
- There are a range of clocks and watches available, designed specifically for people with dementia. These clocks tell the time in a simple digital format and/or can often speak the time.
- If the person you support is used to traditional clock faces, it can be a good idea to introduce this type of clock or watch early on, so that the person can become familiar with the item.
- Wearing a familiar watch can help with time-keeping. It may give the person comfort by being able to checking it, even if they sometimes find it difficult to read it.
- Try using different ‘reminder’ systems by setting alarms on watches and clocks as a way to remind someone to do things, for example, to take a medication.
- Smart phones can be helpful to set alerts and prompts.
- Make use of a white board in the home, writing reminders about what happens at what time. For example, ‘Get lunch out of fridge at 12 o’clock’ or ‘Fiona will ring you tonight at 7 o’clock’.
- Notepads and post-it notes can also be used to remind the person of things throughout the day that have already happened. For example, ‘You had fish and chips for lunch at 12pm today’.
- Using a clear, large font can help make notes easier to read.
- Consider keeping a notepad and pen accessible, to record who visited and when or to simply write reminders in.
- You may be able to use devices such as Alexa (home based personal assistants) to send reminders.
- Sometimes visual prompts can help signal the time of day, such as leaving out a set of clothes in the morning and nightclothes in the evening.
- If possible, try to keep a window view of the sky/outside available.
- When caring for someone who has been practicing their faith with fixed prayer times, you may notice that they seem agitated at prayer time. They may seem agitated even if they can’t remember how to pray. Be sensitive to their lived experience and religious preferences. Then you can support them as needed.
- Time may also be important in some faith groups where they keep fasts, such as in the Muslim communities. Someone with dementia is not expected to keep their fasts, however if they have always fasted, they may worry about eating or drinking. This may happen if people around them are fasting or talking about it, or from the mention of Ramadhan. Again, be sensitive. Work with the individual.
- Repetitive questions about what the day is or when something is going to happen can feel very draining to respond too.
- For some people with dementia, it may feel like it’s the first time they have asked the question. Try to respond as if you are answering for the first time. Telling the person that they have asked this question many times before may lead to upset and confusion.
- Some people with dementia can become fixated with time. They may ask repeated questions about where they are and what time or day it is. This can be hard to deal with. Talking it through with other carers or care professionals can be helpful.
