The information provided on this page is available to download as a printable booklet.
Food and drink are a source of great pleasure in the lives of many people. Preparing food and taking part in social activities around food and drink are central to family and community life. Dementia does not diminish this but as the dementia progresses the person may require more support to enjoy food and drink related activity.
There is no specific diet for dementia but people are encouraged to eat healthily. Some illnesses or disorders that the person experiences in addition to their dementia may drastically change eating habits. Some dementias can impact on the person’s ability to chew and swallow certain foods.
Assisting someone to eat and drink can feel very uncomfortable at first. Give yourself time to learn this skill. To do this it is important to take time to learn, plan and find out what works best for you both.
This page provides guidance and practical tips on supporting the person with their eating and drinking.
This page covers:
- Establish a routine
- Drinks and fluid intake
- Religious and ethical issues relating to food and drink
- Cups, plates and equipment
- Health conditions that can lead to eating and drinking difficulties
- Additional resources
Establish a routine
People often develop their own eating and drinking routine over a lifetime, so understanding these patterns can be helpful in providing effective support.
- Try to get to know the persons usual habits. What do they like to drink at different times of the day? Do they have one big meal or snack through the day? What are favourite foods and what are foods they really dislike?
- For some people, a routine is less helpful. Being presented with food at set times might not fit in with how hungry they are feeling. Be prepared to abandon routine and offer food when the person is hungry and looking for food regardless of what time it is.
- Having fruit and other healthy snacks available and easily accessible is a good idea.
- People’s habits can change progressively as they age in that people often report preferring smaller portions.
- People also report preferring stronger, saltier or sweeter tastes as they get older.
- Some dementias change people’s sense of taste, so they my start liking strong tasting foods e.g. curries, that they might not have enjoyed previously.
- Understanding how people like to eat their food at different times of the day is important too.
- Do they like to sit at a table or do they prefer a tray on their lap? This may vary at different meal times and whether the person has company or not.
- What things during the day help to trigger the recognition that it is meal time? If the person has the TV or radio on, it may be that meal times are triggered by particular programmes.
- Getting to know these things early on can be very helpful if the person becomes very dependent
Top tips for making it easier to eat and drink well at home
It may be by establishing a good routine that the person can manage their own food and drink. There are several practical things that can make this easier.
- Finger food and eating with ones hands is something that most people have done all their lives.
- Sandwiches, little patties, cubes of cheese and biscuits are easy to eat.
- Healthy snacks, fruit, nuts, olives, jellies can be left in bowls for the person to access.
- Likewise having a jug with a drink in that the person can help themselves to may help.
- A side table next to the person which is clearly in their sight line with food and drink available may be helpful.
- Labelling the food cupboard or fridge my prompt people to help themselves.
- Sometimes people become messier in their eating habits. Try not to comment on this. Together it may be worth discussing using a big napkin whilst eating if this becomes an issue.
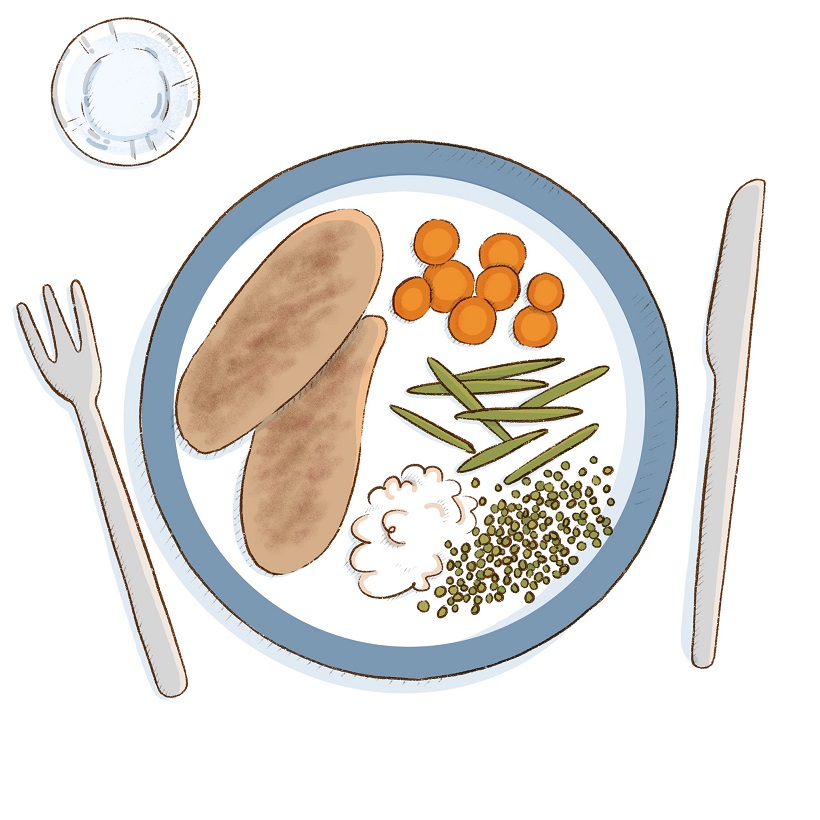
- Dementia can affect a person’s ability to distinguish things that look similar such as white food on white plates on white table cloths. If possible, use contrasting colours for crockery and the table top.
- Heavily patterned surfaces can cause visual issues for some people with dementia. So try and use plain table cloths and crockery.
Top tips for supporting someone to eat and drink
As a person’s dementia progresses, their ability to eat a meal on their own may diminish. The person you are caring for may not be able to identify the food or work out how to eat it.
- Use reminders and cues that it is time for food that you have established in your routine. For example “Well that’s the end of the news. I’m ready for lunch now!”
- Involve the person where possible in preparing the meal.
- This could be in the actual cooking such as preparing vegetables or stirring soup. People are often keen to eat what they have prepared.
- If the person is able, ask them to get the plates out or to set the table.
- Describe what it is that you are going to eat and also describe what is on the plate in from of them.
- Prepare some foods that can be eaten with the fingers.
- Food that can be eaten with breads to mop them up or with a spoon can also be enjoyable.
- Cutting food up can be problematic for many. Cutting food into bite sized chunks may mean that the person can use a fork to eat.
- Sometimes if you start the person off with the activity of eating, they may be able to complete it themselves once they get going.
- If the person doesn’t seem hungry or doesn’t eat much at meal times, offer food in between meals.

Top tips for supporting a person who can no longer eat or drink unaided
Some people who are living with advanced dementia or who have other health issues may no longer be able to eat or drink unaided. Some people may only be able to manage a soft diet or will need their food pureed. Your GP may be able to refer you to a specialist Speech and Language Therapist who also specialise in advising people with chewing and swallowing problems.
- Try to keep to the routines around mealtimes and use the food that you know they like to eat.
- Make sure that both you and the person you are helping are in a comfortable position for eating.
- Have everything you need to hand.
- Describe what the food is and make it sound appetising.
- Load a little of the food onto the spoon and touch the person’s lips with it.
- Encourage them to hold the spoon with you – put your hand over theirs. This will help them to realise that they are eating. It will also help you regulate when they are ready for the next mouthful.
- Allow plenty of time between mouthfuls and watch to see that the person is actually swallowing before you give them the next spoonful.
- If the person is coughing or choking when eating and drinking then a referral to a Speech and Language therapist can be particularly helpful. This can be made through your GP.
Drinks and fluid intake
Drinking plenty of fluids is vital for health and wellbeing.
- The general advice for adults is 2 litres of fluid per day. This will vary from person to person depending on their general health. Seek advice if you are unsure.
- When putting a cup to their lips, place your hand over theirs so they raise their hand to their mouth at the same time.
- Allow plenty of time to swallow.
- Encourage food with high water content such as ice lollies and jellies.
- Some people will still enjoy alcohol. Check that it is ok to have alcohol with any medications the person maybe taking.
- If the person needs to restrict their alcohol intake there are now a wide range of alcohol free or reduced alcohol beverages that can be enjoyed.
Religious and ethical issues relating to food and drink
A number of religions have beliefs about which food and drinks are acceptable and how food should be prepared, such as meat that is strictly halal or kosher. People may also have chosen to restrict certain foods, such as those following vegetarian or vegan lifestyles.
Individuals will vary on how strict their adherence will be to their beliefs. This is up to the individual of course. There may come a time when the person wants to eat something that goes against these beliefs or is given something to eat that is against them. If the person no longer has the mental capacity to make such decisions, it may fall to the carer to decide.
This is something that is important to discuss as part of an Advanced Care Plan and for Lasting Power of Attorney for health and welfare to provide guidance as to what is in the person’s best interests.
Cups, plates and equipment
By and large people will be happier using the eating and drinking utensils that they always have. There are a wide variety of special cups, plates, bowls, cutlery, tables etc. that have been developed for adults that find eating and drinking a challenge. It’s best to try before you buy if you can, or get advice from an Occupational Therapist or dementia specialist.
In the following short clip, Paul shares his experiences of trying to find a suitable drinking cup for his wife to use. Please note this clip is not endorsing any specific products, but showing what did or did not work for Paul and his wife in their situation.
Health conditions that can lead to eating and drinking difficulties
There are many physical health problems that affect appetite. Also if a person is low in mood or depressed they may experience appetite disturbance.
- If a person goes off their food it is worth getting them checked over by a health professional.
- Also do not forget teeth and mouth pain. Toothache or a sore mouth will cause people to not eat and drink.
- You may also need to be mindful of issues such as high blood pressure or diabetes which will restrict the intake or timing of certain foods.
- Some medicines may need to be taken before meals, whereas others need to be taken after eating.
Additional resources
For detailed guidance we recommend accessing the Eating and Drinking Well with Dementia: A Guide for Family Carers and Friends, available to download from the Bournemouth University website www.bournemouth.ac.uk/nutrition-dementia
Alzheimer’s Society showcase a range of eating and drinking aids, you can find them on the shop section of their website shop.alzheimers.org.uk
The University of East Anglia project Drinkit has lots of ideas for how to increase fluid in people’s diets www.uea.ac.uk/groups-and-centres/uea-hydrate-group/drinkit
